If you’re struggling with a burnout, it’s important to take good care of yourself. This means developing a healthy lifestyle. By taking good care of yourself and your body, you can tackle a lot of the cognitive complaints. When we refer to lifestyle, we mean sleep, exercise and nutrition.
Sleep
Almost all people experiencing a burnout have sleeping problems, especially when it comes to falling asleep. The exact relation between sleep problems and burnout is unknown, but it is possible that sleep deprivation and sleep disturbances contribute to the feeling of exhaustion. Sleep deprivation and sleep disturbances can be caused by the excessive production of the stress hormone cortisol, which inhibits your sleep. To limit your cortisol level (especially in the evening), it is important to relax sufficiently, for example by doing breathing exercises, taking a walk or reading a book. In addition, it is beneficial to soak up enough daylight during the day. Daylight inhibits melatonin production during the day and gets it going again in the evening. Melatonin is an important hormone for falling asleep.
Exercise
When you are burned out, you may find physical exercise too intensive. For this reason, it is beneficial to gradually build up your physical fitness. The fatigue symptoms that accompany a burnout are partly due to loss of muscle fitness caused by a reduction in exercise. Therefore, it is beneficial to incorporate small physical activities and moments of rest into your daily schedule. This schedule can be gradually developed step by step in order to rebuild your physical condition. It is important to be active at the scheduled times and rest, regardless of whether you are experiencing any symptoms. By doing this, you will slowly build up a daily rhythm.
Nutrition
Healthy food is important to feel good both mentally and physically. Burnout is often the result of a lack of energy. Energy is needed to recover and continue with your daily activities the next day. Food that provides this energy contains vitamins and minerals. Magnesium, vitamin B12 and omega 3, for example, are very good for the brain. Magnesium can be found in nuts, seeds, green leafy vegetables and whole grains. Vitamin B12 is only found in animal products such as eggs, meat and dairy. With a vegan lifestyle, it is recommended to take a B12 dietary supplement. Omega 3 can be found in fatty fish, walnuts and healthy oils, such as linseed oil.
By adopting a healthy diet, you can support your recovery. For example, answer the following questions when you plan your diet:
What does your eating pattern look like? Are you eating healthy and getting enough vitamins? Do you drink too much coffee? Do you moderate your alcohol intake? Do you eat and drink regularly? Do you take enough time to enjoy a proper breakfast, lunch and dinner and to chew your food well? Are you eating too much sugar?
More information about lifestyle can be found in this article or in the lifestyle library.
Sources:
https://www.gezondheidsraad.nl/documenten/adviezen/2017/08/22/beweegrichtlijnen-2017
https://www.voedingscentrum.nl/encyclopedie/bewegen.aspx
https://www.hersenstichting.nl/dit-doen-wij/voorlichting/gezonde-hersenen/slaap/
https://www.voedingscentrum.nl/nl/gezond-eten-met-de-schijf-van-vijf.aspx
https://www.thuisarts.nl/gezonde-levensstijl/ik-wil-gezond-eten
During treatment of a burnout, you will work on reducing chronic mental stress, improving your physical condition, researching personal goals and getting started with relapse prevention.
The treatment of your burnout is goal-orientated and specifically tailored to your complaints and situation. With the help of your therapist, you will think about goals and start working on your recovery step by step. By carrying out exercises, you will work towards your goals in your daily life.
The treatment consists of different elements, which may vary depending on your personal situation. With the help of your professional, you will assess whether these components are relevant to your situation.
1. Inventory of symptoms
2. Reducing symptoms
3. Cognitive therapy
4. Returning to work
5. Work-oriented interventions
6. Relapse prevention plan
Inventory of symptoms
During this stage, you will create an overview of your symptoms and complaints. What is bothering you? When do these symptoms occur and when did they arise? Do your complaints prevent you from engaging in your hobbies or social activities?
Reducing symptoms
You will work on reducing mental stress and tension (with the help of relaxation exercises, for example). The goal is to improve your lifestyle regarding exercise, sleep and nutrition, too. You will also check whether you have a clear and realistic daily structure.
Cognitive therapy
With the help of cognitive therapy, you will gain insight into your thoughts, feelings and behaviour. These three factors can play a role in the development of a burnout. For example: ruminating about incidents, things that have been said, blaming yourself or working overtime is common among people with a burnout. The goal is to process unpleasant feelings, such as sadness, injustice or anger.
Returning to work
With the help of your therapist, you will create a plan to identify pitfalls and old habits, increasing your chances of a successful reintegration. You may return to work before your symptoms have completely disappeared, which can give you even more insight into your complaints. By doing this, you can practice your new behaviour.
Work-orientated interventions
During this part of the treatment, you will become aware of the alignment between you as a person and your work and learn how to improve this alignment in both the short and the long term.
Relapse prevention plan
You will create a relapse prevention plan with your therapist, in which you will write down, amongst other things, how you can recognize a possible relapse in time and what you can do to prevent an actual relapse.
Source:
Keijsers, G. P. J., Van Minnen, A., Verbraak, M., Hoogduin, C. A. L. & Emmelkamp, P., (2017). Protocollaire behandelingen voor volwassenen met psychische klachten
Burnout is the exhaustion of body and mind due to years of high work pressure or stressful (work) conditions. People who are perfectionist or ambitious run a relatively higher risk of getting a burnout. Similar complaints can also arise from stressful situations that have nothing to do with work, for example when dealing with a long-term relationship or family problems.
What are the symptoms?
Burnout occurs when all three criteria below are met:
1. Chronic stress
A. Chronic stress occurs when at least three of the following symptoms are present:
-
- Fatigue
- Disturbed or restless sleep
- Irritability
- Difficulty tolerating crowds or noise
- Emotional instability
- Worrying thoughts (e.g., about shortcomings or about the complaints themselves)
- The feeling of being in a rush
- Concentration problems and/or forgetfulness
B. Feelings of loss of control and/or powerlessness occur because stressful situations and/or people can no longer be managed or tolerated.
C. There is a major disturbance in their work or social functioning.
D. The complaints are not a direct result of another psychiatric disorder.
2. The complaints started more than 6 months ago.
3. Feelings of tiredness and exhaustion are paramount.
Although burnout often occurs at work, it does not always have to be work-related. In principle, any situation with high stress and an inability to manage it sufficiently can lead to a burnout. Some examples are students that deal with a high study load or care workers that are under high pressure.
A burnout is the exhaustion of your body and mind due to a long period (years) of high work pressure or stressful (work) conditions. An example of this could be high demands at work, insufficient coordination between person and work or persistent tension in the workplace. Perfectionist or ambitious people are especially at risk of becoming burned out. Similar complaints can also arise in other stressful situations that have nothing to do with work, for example when dealing with long-term relationship or family problems.
Chronic mental stress leads to exhaustion. Biological processes play a major role in this progression. When a particular biological process is repeatedly activated, such as the production of stress hormones, it has consequences on our brain, which adapts to the new environment over time. As a result, your ability to deal with stress decreases over time and you feel an increased resistance to mental effort. You experience this increased resistance to mental effort as fatigue.
How do you feel when you are burned out?
When you are burned out, you feel exhausted or overtired. You can barely work anymore. Nonetheless, people suffering from burnout often continue to work until they are no longer able to. Afterwards, you will probably come to the realization that you’ve been struggling with work for some time. Your overactive stress system makes you feel less alert, you can’t handle as much stress as before, your concentration and your memory deteriorate. You may also suffer from headaches, sleeping problems and hypersensitivity to stimuli, crowds and noise. Often, you won’t have the energy to do activities and you struggle to make an effort. You may struggle to motivate yourself and can experience low moods. It can be very difficult to recover from this on your own. Would you like to read more about the diagnostic criteria and the symptoms associated with a burnout? You can find more information in this article.
What are the risk factors for developing a burnout?
A burnout is caused by an interaction between (working) circumstances and personal characteristics. At work, you may have to deal with high work pressure, conflicts in the workplace, (too) little control or uncertainty over what is expected of you. In terms of personal characteristics, being over-involved in your work and having difficulty saying ‘no’ can significantly contribute to feeling burned out. You may be a perfectionist and a hard worker. As a result, you are often occupied with work outside of working hours, you struggle to take criticism and become irritated when something does not go according to plan.
Treating a burnout
During the treatment of a burnout, you and your therapist will look at tension and relaxation, lifestyle, thoughts and situations that contribute to your complaints and your work environment. You will learn to know your limits and boundaries and how you can set them. You can read more about what the treatment will look like in this article.
Source:
Keijsers, G. P. J., Van Minnen, A., Verbraak, M., Hoogduin, C. A. L. & Emmelkamp, P., (2017). Protocollaire behandelingen voor volwassenen met psychische klachten.
During your grieving process, you may have the tendency to isolate yourself and become less active. Grief can be accompanied by depressive symptoms such as a depressed mood, decreased motivation and difficulty sleeping. This can make activities seem less enjoyable. Or the loss may make it more difficult practically to participate in some of these activities. However, even though it may not seem like it now, the activities that used to be important to you and made you feel good are more important than you think. They can positively contribute to your grieving process. Participating in activities can help to properly process your loss.
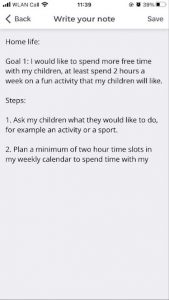
This exercise is intended to help you take the first steps to becoming more active. You will do so by setting tangible goals, also called SMART goals. A SMART goal is one that is Specific, Measurable, Acceptable, Realistic, and Time-bound. For example, not “I would like to socialize more”, but “I would like to start meeting my friends again (specific) at least once a week (measurable and realistic) by the end of the year (limited in time and acceptable)”. Creating a SMART goal makes it more tangible; the goal is clearer, you are more focused and will therefore be more motivated. This can help you to formulate specific steps and actions to achieve your goals.
How can I do that?
Write down your personal goal for each of the categories below:
- Home life
- Work
- Education
- Health/Vitality
- Social activities
- Recreational activities
Then write down three steps that will help you to achieve these goals.
Below, you can find an example.
Source:
When you experience a loss and go through the process of grief, the emotional experience can be very intense. The emotions can be painful, or you can be afraid to let them in. Therefore, you may start to avoid the emotions, thoughts and reality surrounding the loss, and push them away. However, it is important that you make room for these emotions of sadness or anger and acknowledge your feelings. Avoiding them can cause the grief to become more intense in the long run and make it more difficult to eventually let go of these corresponding emotions.
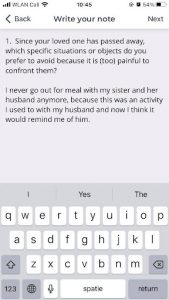
This exercise will help you recognize these emotions and accept the reality of your loss, so that you can move through the grieving process. This requires that you gain insight into the things that you do to avoid the grieving process, so that you can confront them in the future with support from your social network or professional.
Use the questions below to indicate which avoidance behaviour you are prone to rely upon.
Avoidance of the reality of loss
- What are the consequences of the loss that you would rather not think about?
- What are feelings you would rather avoid (for example, anger, sadness, or guilt)?
Avoidance of specific situations or objects
- Since your loved one has passed away, which specific situations or objects do you prefer to avoid because they are (too) painful to be confronted with?
Avoidance of memories of specific events
- Are there specific events related to the loss that you would rather not think about because they are too painful?
- Are there certain memories that give you anxiety that you would rather push away?
Avoidance of giving up grieving behaviour
- What do you do to keep your deceased loved one close and/or to avoid having to think about the fact that he or she is not coming back?
Example:
Source:
Keijsers, G. P. J., Van Minnen, A., Verbraak, M., Hoogduin, C. A. L. & Emmelkamp, P., (2017). Protocollaire behandelingen voor volwassenen met psychische klachten.
There are various types of therapy that can be relied upon for the treatment of dysthymia. Sometimes, they can be effective when followed individually, but they can also be combined. The treatment of dysthymia has many similarities with the treatment of depression. Below, you can find an overview of some of the therapy options:
- Cognitive Behavioural Therapy (CBT): This is an integration of Cognitive Therapy and Behavioural Therapy. You will investigate the thoughts and behaviour that sustain your complaints and learn techniques to change them. For a more in-depth explanation of CBT, check out this video. To get a better idea of what Cognitive Therapy entails, you can find further information here.
- Interpersonal Psychotherapy (IPT): With this type of therapy, the focus is on social aspects. When you’re suffering from depression, you are often dealing with a disturbance in your social environment. A conflict with someone, for example, or a lack of social contact, which leads to loneliness. You can find more information on IPT here.
- Pharmacological treatment: When you are suffering from depressive symptoms, you are dealing with a disturbance that affects the hormones that influence your mood and feelings, such as the neurotransmitter serotonin. Medication can provide support by reducing the intensity of your symptoms. Research has shown that medication is very effective. The combination of therapy and medication has also shown great results. You can read more about antidepressants here.
- Mindfulness: Mindfulness combined with Cognitive Therapy has proven to be an effective combination. During this type of treatment, the focus is put on negative thinking patterns or unhealthy habits such as worrying. By practicing meditation, amongst other things, you learn to recognize these unhealthy negative and/or recurring thinking patterns and disconnect from them. Mindfulness reduces worrying and reduces the risk of relapse. You can read more about what is meant by mindfulness here.
Sources:
Psychotherapy for chronic major depression and dysthymia: a meta-analysis P Cuijpers, A van Straten, J Schuurmans, P van Oppen, SD Hollon, and G Andersson. https://www.ncbi.nlm.nih.gov/books/NBK77927/
Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study Thorsten Barnhofer, Catherine Crane, Emily Hargus, Myanthi Amarasinghe, Rosie Winder, J. Mark G. Williams
https://www.sciencedirect.com/science/article/pii/S0005796709000333
Rumination as a predictor of relapse in mindfulness-based cognitive therapy for depression Johannes Michalak∗, Anne Holz and Tobias Teismann
https://pubmed.ncbi.nlm.nih.gov/22903859/
Dysthymic disorder is also known as dysthymia, chronic depression or persistent depressive disorder. Dysthymic disorder can be diagnosed when you experience a low mood almost every day for at least two years. Dysthymia can also be seen as a mild form of depression, in which symptoms are present to a lesser extent and lower intensity. This can make it difficult to realise that you are suffering from a form of depression. With dysthymic disorder, it can feel like you’ve always been like this; you don’t know any different from feeling low. However, people with a dysthymic disorder suffer no less than people that suffer from ‘normal’ depression. You can feel very lonely and unhappy, and your complaints can affect your ability to function on a daily basis.
What are the symptoms associated with dysthymic disorder?
The main characteristic of dysthymic disorder is that you have experienced low mood for the majority of the time for over two years. In addition, you struggle with at least two of the following symptoms:
- You feel sad, anxious or empty.
- You have a lower interest in pleasurable activities.
- You notice a change in your appetite; you have lost or gained weight.
- Your sleeping pattern has changed; you have trouble sleeping or sleep less or excessively.
- You notice changes in your activity levels; you feel restless and/or move more slowly than usual.
- You are mentally and physically tired.
- You experience feelings of guilt, helplessness, worry and/or fear.
- Your self-esteem has decreased.
- You have concentration problems and difficulty making decisions.
- You have thoughts about death and/or suicide.
Long periods of low mood can alternate with periods during which you feel better. These periods often last no longer than two months. When suffering from dysthymia, you therefore feel depressed for the majority of the time. The disorder often occurs in combination with other psychological disorders, such as an anxiety disorder, a personality disorder or an (alcohol) addiction.
The difference with a ‘normal’ depression
As mentioned above, dysthymic disorder is similar to major depressive disorder. The difference is that you suffer from fewer symptoms and your complaints are less intense. However, the symptoms are present for much longer than with a ‘normal’ depression. It is possible to have both a depressive disorder and dysthymia, which is the case when you normally have dysthymic symptoms, but also occasionally have additional symptoms that make you temporarily meet the characteristics of depression. We then refer to depression in combination with dysthymic disorder.
You can read about the treatment of a dysthymic disorder in this article.
Sources:
Mentaal Beter, Lentis PuntP, MindBlue, depsycholoog
What is depression?
There are various psychological and physical symptoms that are associated with depression. These symptoms can influence the thoughts and behaviour of someone suffering from depression. Not everyone who suffers from depression experiences the same symptoms or experiences them to the same intensity. In most cases, you can refer to depression if a low mood lasts for a long period of time. Depression is almost always associated with low mood and a reduced pleasure/interest in activities that someone would normally enjoy. In addition, they often experience changes in appetite, sleeping pattern, concentration and self-confidence. A less common form of depression is bipolar depression. A person suffering from bipolar disorder alternates between periods of depression and very eccentric periods during which they feel good, but behave abnormally. This can manifest itself in, for example, substance abuse or rash expenditure of money. Such an abnormal period is also referred to as a manic episode.
What does someone with depression experience?
Psychological complaints can include feelings of guilt, worthlessness or powerlessness, anxiety and crying. Physical complaints can include fatigue, little to no appetite, poor sleep, dry mouth, pain, tightness of the chest, dizziness, heart palpitations. Thoughts and behaviour can include irritability, suicidal thoughts, excessive worrying, forgetfulness, indecisiveness, thinking or reacting slowly and restlessness. As you can imagine, a combination of the complaints listed above can be a heavy burden. Someone suffering from depression often has difficulty performing daily tasks, such as housekeeping, shopping and/or administrative tasks. Furthermore, someone suffering from depression often struggles with passivity and, therefore, rarely initiates or takes action. Guilt can also play a big role in depression. For example, someone can feel like a burden to their social circle.
What does someone with depression need?
As a partner, family member or friend, you can support someone with depression. By listening and empathizing with the other, you can show support. Offering help in the areas that someone is struggling with can be valuable. You can also provide support by, for example, attending a meeting between them and their doctor or therapist. Talk to the other person about how you can best offer them support. For example, ask whether he/she has drawn up a relapse prevention plan during his/her treatment and whether you can have a look at it. By doing this, you can discuss which signals to look out for and point out whenever things seem like they are not going well with the other person.
What can you do?
- Keep in contact with each other regularly. This is one of the most important things. It shows that you are involved and that they can contact you.
- A conversation with a doctor or therapist can be difficult. You can support someone by coming along if they would appreciate the support.
- Support them without judgment or disapproval. Try to do so with patience and warmth. Encourage and motivate the other in an understanding way.
- Realize that the other has and must keep control. Do not exert too much pressure and do not (try to) take over control, that is counterproductive. Avoid being too accommodating, either. Be a good example to the other, this can inspire them to act in the same way.
- Learn about depression so you can understand what someone is going through in a better way. Further information can be found in the NiceDay Mood complaints library or on the MIND and Thuisarts
- Having a structured day is very important for people with depression. For example, you can help them to create a daily schedule with certain activities so that it is easier for them to stay active.
- Provide them with help with daily tasks if possible and if they would like that. Daily tasks, such as grocery shopping and housekeeping, can sometimes be daunting for them.
- Someone suffering from depression may also have thoughts surrounding death or suicidality. Do you notice your friend or partner experiencing these thoughts? Talk to them about it and together contact their practitioner, the General Practice Center (ask for the crisis service) or 113, the suicide prevention line.
What not to do:
- Criticize them. That can make someone feel insecure.
- Pressure them to do something when they are not ready for it.
- Tell the other person what is wrong with them or what they are doing wrong. Therefore, do not lecture or advise them on what they should or should not do.
- Try to solve their problems for them. Avoid minimising or downplaying their problems. Take them seriously and pay attention to the problems.
- Take on the role of therapist.
Take care of yourself
As a partner, family member or friend, you can end up going through a difficult time yourself. That’s why it’s important to take good care of yourself. Make sure that you do not become overburdened in caring for your partner/friend/family member that is suffering from depression. It is understandable if you find it difficult to deal with their symptoms/complaints. You can prevent yourself from becoming too stressed out by continuing to do enough enjoyable and relaxing things yourself. Keep in touch with a good friend, someone to whom you can vent and talk about your problems. Is it all getting a bit too much? The Depression Line (088 – 505 43 34) or the Depression Association can also provide you with support and someone to talk to. It can also help to come up with practical tools that can help you or your partner/friend/family member in certain situations, so that you know what you can (and cannot) do for the other person.
Sources
MIND blue: Info en tips naasten depressie
Manja de Neef, Negatief Zelfbeeld, BOOM
PsyQ: wat kun je doen als naasten?
MIND: depressie brochure naasten
Thuisarts: hoe ondersteun ik iemand met psychische klachten?
Before completing the treatment, we will discuss identifying and preventing similar complaints in the future.
Experiencing complaints again is normal, so see this as a reassurance plan. Fortunately, experiencing complaints again does not mean that you are back to square one, it can actually help you to see that something is going on and inform you on how to intervene before you relapse.
To ensure that your complaints do not worsen, it is important to be able to identify when you are feeling low or when you begin to revert back to old patterns early on, so that you can intervene in time. This document can help you with this and help you create a relapse prevention plan or reassurance plan.
It consists of three steps:
Identifying, repeating and seeking support. It is advised to regularly read this form after completing your treatment and keep it nearby.
Step 1) Signals and risk situations
It is important that you can identify or recognize when you are feeling low. Some people notice this in their bodies, others notice this in their behaviour.
What signals are you aware of that indicate that you aren’t feeling well?
We can subdivide these signals into:
- physical signals: e.g., back pain, headache, lethargy
- psychological signals: e.g., worrying, concentration problems, negative thoughts
- behavioural signals: e.g., sleeping badly, withdrawing, no longer exercising, drinking more alcohol, working too hard, getting angry faster
Fill in the list below. Think back to the period leading up to the complaints. Describe the signals as concretely as possible. Examples of this are: “Lying awake in bed for more than an hour a day for a week” or “Coming home from work exhausted for two weeks’’.
Physical signals:
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
Psychological signals:
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
Behavioural signals:
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
Risk situations
In addition to recognizing signals, it is also important to recognize circumstances that can increase the risk of a relapse, so-called ‘risk situations’.
Examples are: busy weeks at work, arguing with family, conflicts at work, moving to a new house, having to work night shifts, ending a relationship, disappointment, etc. Based on the presence of risk situations, you can decide if extra interventions to prevent relapse are needed. Describe the risk situations that are relevant to you.
______________________________________________________
______________________________________________________
______________________________________________________
______________________________________________________
______________________________________________________
Step 2) Practising what you have learned
People learn through practice, such as learning how to ride a bicycle or learning how to skate, which probably started as trial and error, but eventually got better and better! It is therefore very useful to repeat the most useful elements of the treatment by writing them down below. We use the terms ‘pitfalls’ and ‘tools’.
Pitfalls
Pitfalls are thoughts that are or behaviour that is not helpful, but that you tend to rely upon when you are feeling unwell. These are, for example, thoughts such as “I am not important” or behaviour such as withdrawing instead of seeking support.
Enter below what you tend to think when you are not doing well and how you are inclined to behave when you are not doing well.
Pitfalls – Thoughts or Beliefs
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
Pitfalls – Behaviour
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
Tools
Tools are ways, methods or techniques that you can use to deal with difficult situations or thoughts. Think of everything you have learned during your treatment, but also of things that you have discovered and experienced as helpful during this recent period. Write them down below.
Some examples are comforting yourself, talking to others, challenging thoughts with a thought record, anti-anxiety exercises, relaxation techniques, rest, exercise, etc.
Tools – That help me when I’m having a hard time
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
___________________________ ___________________________
Step 3) Get support or help
During the treatment process, you may be able to recognize the individuals who can help you when you are feeling down. Write down below who these people are and what they can do for you. For example: someone with whom you can talk, someone with whom you can laugh, someone who can motivate you, someone who does not judge you, etc.
Who What can this person do for me?
______________ ______________________________________
______________ ______________________________________
______________ ______________________________________
______________ ______________________________________
______________ ______________________________________
Rounding off
Do you have any extra motivational or helpful words for yourself? Think of a saying, a quote that gives you courage or that you find inspiring, or a short letter to yourself.
Write this down below:
______________________________________________________
______________________________________________________
______________________________________________________
______________________________________________________
______________________________________________________
______________________________________________________
______________________________________________________
______________________________________________________

